
Comprehensive Care for Peripheral Vascular Disease at AMC
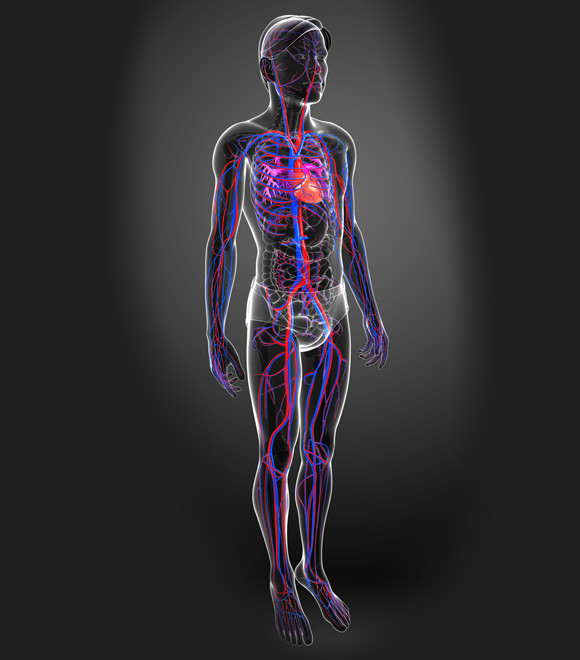
Peripheral vascular disease is a circulatory disorders caused by reduced blood flow to the limbs, most commonly due to atherosclerosis or thrombosis. As atherosclerotic plaques accumulate inside the arteries, the vessels become narrowed, limiting blood supply to the muscles. Risk factors such as diabetes and smoking significantly increase the likelihood of developing these vascular conditions.
At the AMC Peripheral Vascular Disease Center, we offer comprehensive, patient-centered care at every stage of treatment, from accurate diagnosis and medical management to advanced endovascular procedures, complex vascular surgeries, and personalized rehabilitation programs.
Our team of highly skilled specialists provides optimal care through state-of-the-art endovascular procedures and advanced surgical techniques. We operate a fully integrated multidisciplinary system, collaborating with specialists from departments including vascular surgery, cardiology, thoracic and cardiovascular surgery, radiology, anesthesiology and pain medicine, plastic surgery, endocrinology and metabolism, rehabilitation medicine, and intensive care unit. This collaborative approach ensures that every patient receives the highest standard of care tailored to their individual needs.
Treatment options

Patients diagnosed with peripheral vascular disease receive care treated through a combination of risk factor management, exercise rehabilitation, medication, and revascularization procedures, inclduing percutaneous interventions or surgery.
Risk Factor Modification
The main risk factors for peripheral vascular disease include smoking, diabetes, hypertension, and hyperlipidemia. Among these, smoking is considered the most significant contributor. Quitting smoking not only slows disease progression but also lowers the risk of limb amputation and reduces the occurrence of rest pain. In addition, medical therapy combined with lifestyle changes can reduce the risk of peripheral vascular disease as well as related cardiovascular conditions.
Exercise rehabilitation
Exercise rehabilitation is proven to alleviate claudication symptoms and improve patients’ mobility. It enhances vascular endothelial function, reduces oxidative stress in post-ischemic muscles, and promotes angiogenesis, the formation of new blood vessels from existing ones. Regular exercise also helps control risk factors by improving glucose metabolism, lowering cholesterol and triglyceride levels, and supporting efforts to quit smoking.
For optimal benefit, patients are advised to exercise three times per week for at least 24 weeks. Each session should gradually increase to 35 to 50 minutes at an intensity that causes mild discomfort or aching. Long-term management through regular cardiovascular exercise such as walking, cycling, or swimming, combined with strength training, is recommended. Exercise rehabilitation is often the foundation of peripheral vascular disease treatment, improving walking distance by 2 to 2.5 times and significantly relieving symptoms.
Medical Therapy
Antiplatelet agents and lipid-lowering therapies play a key role in managing peripheral vascular disease. These medications help reduce the risk of heart attack, stroke, and death from vascular-related causes in affected patients.
Revascularization
According to the American Heart Association (AHA), percutaneous or surgical revascularization may be considered in the following situations:
- When symptoms do not improve with exercise rehabilitation or medical therapy, or when improvement is not expected
- When claudication severely limits daily activities or quality of life
- When significant improvement is anticipated from relieving claudication
- When the patient’s overall medical condition and prognosis are suitable for intervention
- When revascularization can be performed with low short- and long-term procedural risk
- In cases of external iliac artery stenosis or occlusion
- In the presence of rest pain, ischemic ulcers, or gangrene
Revascularization, whether through percutaneous intervention or bypass surgery, restores blood flow to the affected limb. The choice of procedure depends on the anatomy and length of the lesion as well as the patient's overall health.
